Key Points
- In the emergent data-driven economy, a nation’s collective ability to amass, control, own and commercialize data will determine its ability to provide economic and public benefits to its citizens, due to its fundamentally single-payer system. This system creates an effective mechanism to advance a collective health-data economy.
- Collective health-data assets will benefit clinical decision making, the delivery of personalized medicine, the advancement of artificial intelligence (AI), the acceleration of medical research and much more.
- Further, corporations that own or access the largest parts of the medical information life cycle will be the economic winners — along with their governments.
ove over, knowledge-based economy. Hello, data-driven economy.
Canadians are sleepwalking into a new reality, one that has been exploited successfully by today’s mega firms — Google, Facebook, Amazon, Uber and others — for more than a decade. For most, if not all, commercial firms, data is the critical capital input to tomorrow’s economy.
Innovators and start-ups can develop new intellectual property (IP), but cannot compete on an access-to-data basis with these mega firms. Given their head start in the data-driven economy, mega firms’ deep pockets enable aggressive take-out strategies that eliminate future competition.
Traditionally, Canadian governments have taken an administrative or regulatory stance on the data of citizens. Ambivalent about using data as an economic opportunity, governments have prioritized privacy and security over data’s potential to spur growth. This conservative approach can hinder firms’ ability to capitalize on data as a driver for innovation and growth. But when it comes to data, innovation and wealth generation, governments stand to reap the same economic benefits as domestic commercial firms.
In the data-driven economy, data has properties that are entirely different from how resources have previously been conceptualized. Data, unlike a traditional commodity such as oil, increases in value as it becomes more abundant. This effect can be multiplied almost infinitely when data is combined across multiple distinct data sets. As such, data should be considered not as one asset class, but an infinite series of asset classes, rising and falling in value across multiple dimensions. The consequence is that when making policy, governments will need to consider different sectors in the data-driven economy as individual components of a larger, interconnected domain.
Health care is one of the largest and fastest-growing industries in the world. Within it, there exists a high-stakes interplay of individual rights, collective benefits, levers, obligations and private commercial interests. In the data-driven economy, the collective ability to amass, control, own and commercialize these new assets will determine our ability to provide social services, health care, security and jobs for Canadians.
This essay makes the case for collective action on data use in one sector of the economy — health care — in which Canada has a structural competitive advantage due to the public sector share of spending.
The Data Science of Health Care
Canadian innovation in health care has come a long way from the discovery of insulin in 1921. The conditions that could be treated were poorly understood, and conventional academic approaches to research involved slow and constrained data capture and analysis. Today, rapid advances in technology are changing how we think about health care. The cost of gathering copious amounts of real-time data is declining by orders of magnitude. As revealed by a Dell EMC (2014, 5) study, the volume of this data is growing exponentially (48 percent per year) and is estimated to reach over 2,000 exabytes by 2020, more than one million times larger than the Library of Congress’ data holdings. This data is generated by a growing number of sources, transforming how medical knowledge is created and, in turn, how health care is provided.
This data is generated by a growing number of sources, transforming how medical knowledge is created and, in turn, how health care is provided.
Instead of periodic testing, continuous monitoring of patient disease states will be available. These data-gathering techniques (wearables, implants, bionics, devices, patches and social data) provide health-care professionals with a new set of tools. In lieu of a symptomatic approach to diagnosis and analysis (subjective indications of pain, blood pressure, blood sugar or body temperature), continuous monitoring will provide objective and precise measurements. With this, data from genetic, epigenetic, phenotypic and microbiomic sources can be combined, and disease pathways and the environmental and social impacts thereon will be better understood.
In health care, unlocking the potential value of data will depend on the implementation of new policies, standards and technologies to facilitate open, structured and secure data sharing within a regulatory framework that protects individual rights.
A Case for Canada
The benefits of data interchange include: increasing the operational efficiency of care; better monitoring of emerging epidemiological trends; improved clinical decision making and risk management; delivery of effective personalized medicine; enabling AI application and machine learning; and accelerating medical research. Investments that facilitate access, manipulation and analysis of health-data assets will also generate large amounts of commercial IP. Ultimately, those who own large parts of the medical information life cycle, or those who can access it in order to innovate, will be the economic winners.
While Canadian industry lags behind its southern neighbour in the first generation of industries in the data-driven economy (search, self-driving vehicles, social networks and so on), we have a structural competitive advantage in health care. As revealed by the Canadian Institute for Health Information (CIHI) in 2016, health care is the largest sector of the Canadian economy, representing more than 11 percent of the country’s GDP and approximately 38 percent of an average provincial budget (CIHI 2016, 6; 21). Of Canada’s expected $242 billion health-care expenditure in 2017, 70 percent is funded through its public health-care system (CIHI 2017, 6; 11). This fundamentally single-payer structure creates an effective mechanism to advance a collective health-data economy.
Canada’s predominately public system, and other intrinsic national characteristics that arise from this structure, offers the following competitive advantages:
- The ability to drive policy and standards through procurement. Health-care organizations and governments are required to conduct open procurements for goods and services, which enforce compliance with Canadian data regulations.
- Advanced data access and sharing through centralized health-care systems. Many Canadian provinces and territories directly administer health-care delivery to their populations, which can support better care through effective supply chain management and expansive data collection.
- Pan-Canadian health-care organizations with mandates to set national standards, collect data and accelerate innovation. Organizations such as CIHI and Canada Health Infoway (CHI) collect and disseminate data sets and establish interoperability standards across the country, laying the foundation for an open, collective health-data ecosystem.
- The collaborative spirit of Canadian health care. There is an essential cooperative ethos in Canadian health care, with private sector businesses collaborating to make data intelligible and actionable across multiple siloed information technology systems and vendor products.
- Large, diverse group of Canadian people for population health insights. Canada’s diversity — the genetic, cultural and socio-economic variety of its people — is a rich, variable data pool that can be leveraged (while upholding personal privacy and protections).
- Excellence in AI and machine learning. As a world leader in AI and machine-learning education, Canada has the infrastructure, knowledge and people to develop the world’s most advanced clinical algorithms to sustain health improvement and innovation.

While health care is provincially administered in Canada, with each province or territory responsible for delivering care and managing the health data of its own population, pan-Canadian organizations are uniquely poised to bridge disparate health administrations and drive harmonizing interprovincial and national health-care improvements. A recent example is PrescribeIT, a pan-Canadian e-prescribing service, awarded through a public procurement, which is now compelling national health standards around medication and identity management. Similar approaches are possible for health data, which can empower data standards and interoperability across jurisdictions. The ability to share patient data across provinces is imperative to improving continuity of care and increasing system efficiencies such as reducing wait times, especially in provinces with high volumes of patients receiving out-of-province care, such as in the Maritime provinces.
In Canada, the discourse on data has become a tug-of-war between individual rights and private commercial interests. Governments only had to draw one line — privacy. Once the individual’s privacy rights were encircled through constitutional interpretation and privacy regulation, the rest was left to private commercial opportunity. Canadian governments have traditionally taken an administrative or regulatory stance on the health data of individuals and have shied away from harnessing this data’s economic potential.
To fully consider the policy implications of health data in a single-payer health context, this two-way framework must be extended to consider the collective interest, as distinct from individual and private commercial interest.
A New Social Contract with Citizens
Health data is among the most private and personal of all data. However, a majority of it is not under the deliberate control of the individual. As firms create new ways to exploit personal data, courts and legislatures around the world are extending individual privacy rights and protections. In the European Union, this has recently taken the form of the General Data Protection Regulation (GDPR), which puts significant obligations on firms to protect personal data, including personal health information (PHI). It also provides for individual rights over data and its use, storage and, notably, destruction (described in article 17 as the “right to erasure”).1
As firms create new ways to exploit personal data, courts and legislatures around the world are extending individual privacy rights and protections.
Conversely, the United States maintains low privacy protections for the personal information of foreign citizens, creating a “policy arbitrage” between Canada and the country where a significant portion of Canadians’ personal information is stored. Section 14 of US Executive Order 13768, “Enhancing Public Safety in the Interior of the United States,” states: “Agencies shall, to the extent consistent with applicable law, ensure that their privacy policies exclude persons who are not U.S. citizens or lawful permanent residents from the protections of the Privacy Act regarding personally identifiable information” (The White House 2017). As such, US firms can do more with the personal information of Canadians that is stored in the United States than they can with the personal information of Americans.
As firms use this PHI to generate private wealth, individuals will rightly question their data rights. To that end, any data strategy in health care must begin first with a new social contract between the people providing PHI, the firms that collect it and the governments that pay for it.
While not exhaustive, the following is an outline of principles to be considered in this new social contract, in particular as it relates to the 70 percent of health-care costs paid for by the government:
- The individual must have the right to control their PHI. The health-care system must allow individuals control over their PHI, instead of acting as filters or gatekeepers of that access.
- The individual must have the right to consent to the secondary use of their anonymized PHI. Technology firms should be held accountable for enshrining individual rights of control over secondary use in their systems.
- Firms must disclose to individuals the intended secondary use of their data at the time of consent. However, this should not be as narrow as provided for under the GDPR, as today’s technologists may not understand the potential value for a set of data tomorrow.
- The penalties for privacy breaches should be severe and transparent to individuals. This is especially true in cases of misconduct or negligence.
- Due to policy arbitrage between nations, Canadian PHI should remain in Canada. Until international or bilateral rules are developed, Canadians must look to domestic courts and lawmakers for restitution and enforcement.
Acting on Our Collective Interests in Health Data
To fully understand the need for collective action with respect to health data, one must first understand the important distinction between ownership and control. In health care, where PHI may belong to the individual, control of the data dictates access and secondary use.
As shown in Figures 1 and 2, innovation from data follows a simple pattern, using statistical analysis, machine learning, deep learning and so on.
Figure 1: Singular Control of a Unique Data Set
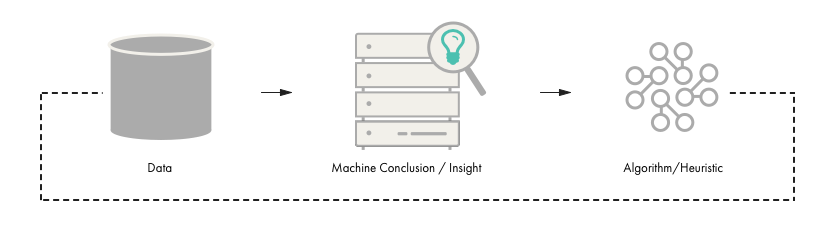
Figure 2: The Exponential Effect of Increasing Data
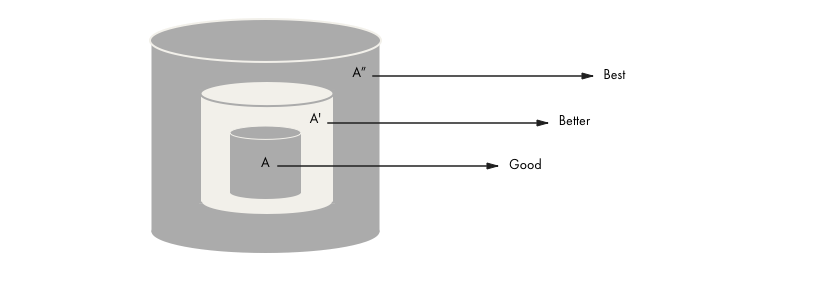
When a single firm controls a unique data set, it can charge high rents for access to the (potentially life-saving) algorithm. As a result, vast amounts of health data remain isolated and underutilized.
Limiting access to data also reduces the possible innovation from that data. More data leads to better algorithms and insights. This effect is multiplied when multiple types of data are combined. Consider Figures 3 and 4, below.
Figure 3: Value of Combining Data Sets
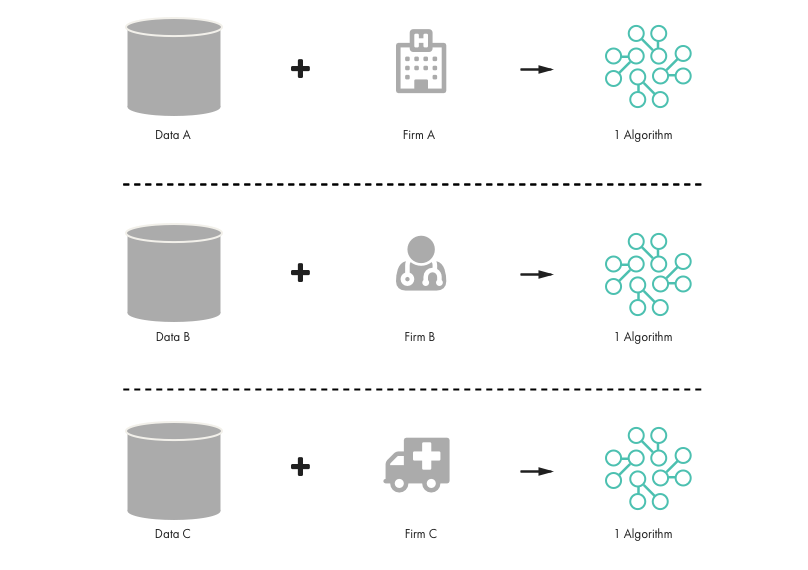
Figure 4: Combining Multiple Data Sets, Multiplying Value and Insights
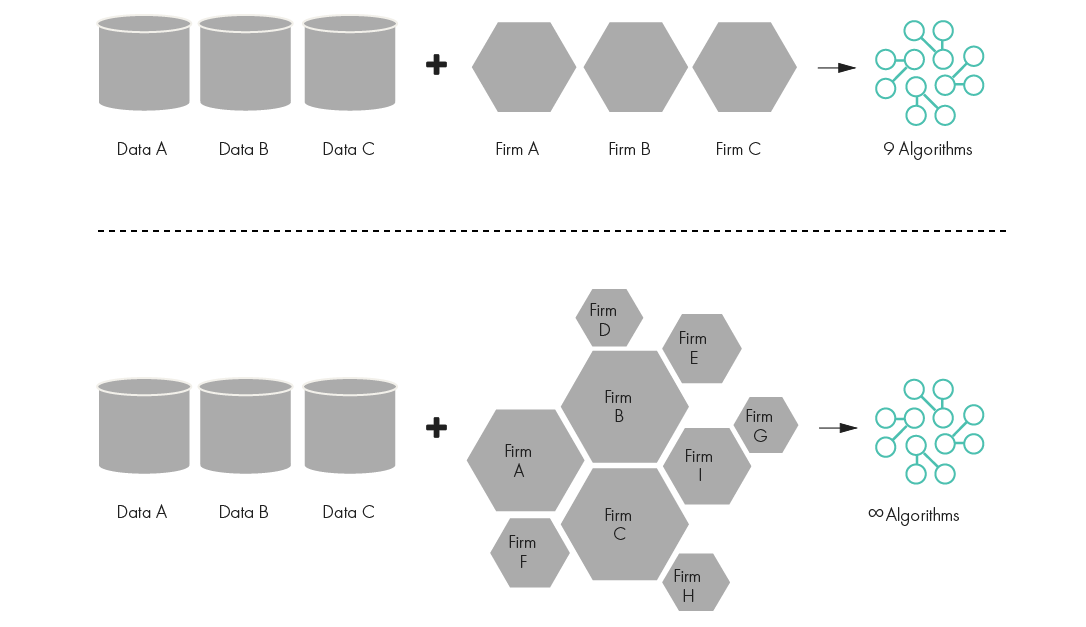
To deliver the best possible care, both large numbers of shared data sets and innovators accessing this data are needed. Canada can capitalize on its strategic position to make this a reality in health care through a thoughtful exercise pertaining to regulations and purchasing power. This might involve the following:
- Use federal and provincial health purchasing power to unlock health data for the benefit of all. Subject to individual rights in opting out, all health data generated as a result of public spending should be made publicly available in an anonymized fashion at zero or nominal cost.
- A rules-based access framework must be created for this data. Firms must demonstrate the ability to securely manage data, perhaps through certification or contractual means.
- Data should be retained for a lifetime or longer. As machine learning matures, previous stores of data will prove valuable in solving problems and yielding potentially life-saving insights.
- Accelerate the development of health-data standards and require that publicly procured technologies conform or adjust to them. The Health Standards Organization and the Standards Council of Canada should be empowered to continuously develop and refine standards.
- Access to this data should follow the principle of benefit to Canadian society. Canadian firms, or firms that provide access to their own data, should gain the greatest benefit. This may lead to variable pricing for access (low for domestic firms and higher for foreign firms).
- Certain uses of health-care data compromise trust in disproportion to their benefit. Access should be subject to regulations that limit certain behaviours. These may include banning the re-identification of individuals using anonymized data and limiting the use of data for activities such as marketing.
An important overlay on this discussion is that of IP. In health care, while data belongs to the individual, and the state can create rules of access for secondary use, the state should not own the IP generated therefrom. Instead, the protection of algorithms created from this data should be incentivized, perhaps using the innovation box or patent box approaches that are deployed in other countries.
Broader Policy Implications
The implications of the data-driven economy in health care will extend far beyond the discussion in these pages. Every aspect of health delivery will be impacted:
- Reimbursement schedules will need to become agile. Regulatory cycles relating to clinician reimbursement will need to be measured in months rather than decades.
- A new approach to regulating data-driven machine algorithms will be needed. The pace of algorithm development will outstrip our ability to understand, regulate and monitor, so we must take a risk-based review and disclosure approach.
- The health-care workforce of the future will be unrecognizable. With machine intelligence, certain clinicians (nurses, pharmacists, physician assistants and personal support workers) will be able to deliver the majority of care. Physicians will consolidate into super-specialists, and there will be a dramatic increase in technicians, engineers and technologists.
Time to Act
To date, Canada has been an observer and rent payer in the data-driven economy. However, in health care, Canada has a clear opportunity to stake out a leadership position. Those who own the largest parts of the medical information life cycle, from data capture to insight to machine algorithms, or those who can access it in order to innovate, will be the economic winners.
The future of health-care delivery will be data-driven, scientific and increasingly personalized. Eventually, the accumulation of data will shift health care from reactive to preventative — adjusting our behaviour, our biome and perhaps even our genome. We can act now, lead in our collective interest and create the foundation to develop world-class data-driven innovations, or we can let this opportunity pass us by and continue to pay rent for our own health data.